Researchers at the Toronto General Hospital Research Institute have discovered that combining novel immunotherapeutics can boost the immune system’s capacity to recognize and kill liver cells infected with Hepatitis B virus.
Hepatitis B (commonly known as hep B) is a serious infection of the liver that can be prevented through vaccination. Unprotected individuals that contract the disease often develop a short-term infection; however, for some, the infection becomes chronic and can lead to life-threatening conditions such as liver cancer or scarring of the liver known as cirrhosis.
Current treatments cannot fully eliminate the virus, so, for some, these treatments may need to be taken life-long to prevent the disease from progressing.
“Patients with chronic infections face a double threat of disease progression: first, the sustained presence of the virus in the body begins wearing down the immune system, making viral clearance a very rare event; second, when treatments are paused or missed, the virus can quickly rebound. The goal is to restore the patients’ immune system so they can clear the virus without treatment” Explains Dr. Adam Gehring.
“In our study, we explored how novel therapeutics—small interfering RNA (siRNA) and immunomodulators—impact the immune system to maximize immunity against hep B virus,” explains Adrian Kuipery, the first author of the study.
The researchers first tested the effects of siRNAs, which are a novel type of antiviral drug that, in this context, stops the virus from replicating but does not eliminate it. The results showed that siRNAs, while slowing the virus, prevented the immune system from recognizing cells infected by hep B virus. “Our findings suggest that siRNA treatments should be carefully timed in combination studies where other treatments, like vaccines, try to boost hepatitis B immunity. You don’t want to boost immunity to the virus and then have the infected cells invisible to the response.” explains Adrian Kuipery.
The research team then looked at immunomodulators, which are drugs that aim to jump-start the immune response by mimicking naturally occurring stimulatory signals for the immune system (e.g., cytokines). “Early clinical trials suggest that immunomodulators alone are not enough to stop hep B virus replication. However, when combined with other immunotherapies, it could boost the activity of the immune system and enhance its ability to recognize infected cells,” adds Dr. Gehring.
“The timing of our study is highly relevant because siRNA and immunomodulator therapies are currently in phase II clinical trials,” says Dr. Gehring. “Our study provides critical insights on how to combine these novel therapies with existing therapies and also highlights areas that need further investigation.”
This work was supported by the Toronto Centre for Liver Disease, the Canada Foundation for Innovation and UHN Foundation. Dr. Harry Janssen is a Professor of Medicine at the University of Toronto, where he holds the Francis Family Chair in Hepatology. Jordan Feld is an Associate Professor of Medicine at the University of Toronto.
Kuipery A, Sanchez Vasquez JD, Mehrotra A, Feld JJ, Janssen HLA, Gehring AJ. Immunomodulation and RNA interference alter hepatitis B virus-specific CD8 T-cell recognition of infected HepG2-NTCP. Hepatology. 2021 Nov 7. doi: 10.1002/hep.32230.
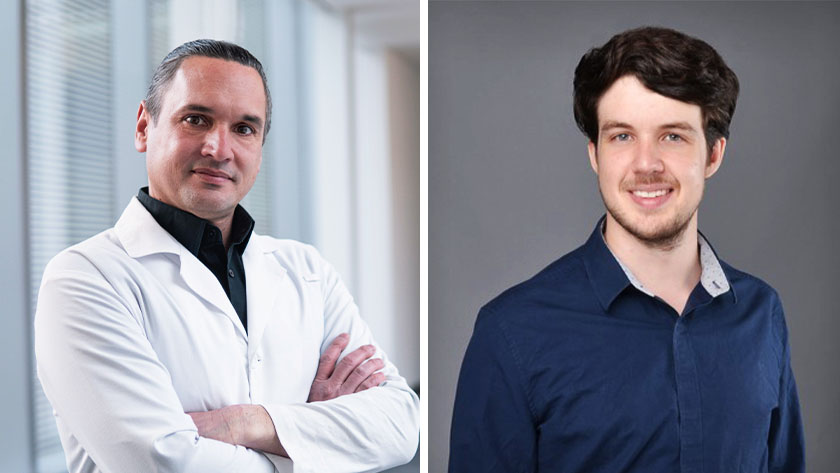
(L-R) Dr. Adam Gehring, senior author of the study, Scientist at the Toronto General Hospital Research Institute and Biology Lead at the Toronto Centre for Liver Disease; Adrian Kuipery, first author of the study and PhD candidate.




