
A study from The Institute for Education Research (TIER) at UHN is shedding light on the challenges that arise when the care of a patient is transferred between staff during an operation—a process known as intraoperative handoff.
“By revealing the factors that negatively impact intraoperative handoff, our findings highlight the need to understand the nature of surgical teams to enhance communication and improve patient safety,” says Dr. Carol-anne Moulton, a Clinician Scientist at TIER and senior author of this study.
During surgeries, intraoperative handoffs are a common occurrence. As staff move in and out of the operating room, there is a risk of communication breakdowns. Surgical safety checklists are currently the only tools designed to improve surgical team communication; however, their effectiveness diminishes throughout the procedure—particularly after multiple handoff transitions.
To identify opportunities for improving the safety of intraoperative handoffs, the TIER research team conducted a two-phase study.
In the first phase, the team looked at current handoff practices to uncover how certain assumptions held by the surgical team might affect communication and situational awareness—an individual or team’s understanding of the situation and environment.
After 38 days of observation in operating rooms and 41 brief interviews, the team compiled the data to identify trends. The findings revealed that handoff practices were not standardized and rarely involved the entire team. Underlying assumptions held by operating room team members impeded effective communication and consequently, their shared situational awareness. These deeply rooted assumptions included the belief that team members are interchangeable and can make handoff decisions without consulting others. Additionally, the hierarchical structure of teams and lack of formalized communication practices further hindered effective communication.
In the second phase, the researchers developed handoff safety tools by assessing the components that were frequently overlooked and posed a threat to team awareness and patient safety. The tools that they developed serve as clinical reminders to enhance team dynamics, bridge communication gaps and facilitate shared situational awareness.
“It is critical to recognize the interdependency of operative teams and address deeply rooted assumptions and social norms,” concludes Dr. Moulton. “Only by considering these factors, can we push the needle towards improved intraoperative handoff safety and provide the best possible care.”
This work was supported by the Physicians’ Services Incorporated Foundation and UHN Foundation. Dr. Carol-anne Moulton is an Associate Professor in the Department of Surgery at the University of Toronto. Her research is focused on creating, supporting and fostering a positive team culture in the operating room.
Ramjaun A, Hammond Mobilio M, Wright N, Masella M, Snyman A, Serrick C, Moulton CA. Beyond the Surgical Safety Checklist: Using Intraoperative Handoff to Facilitate Team Situation Awareness in the OR. Ann Surg. 2023 Mar 13. doi: 10.1097/SLA.0000000000005838. Epub ahead of print.
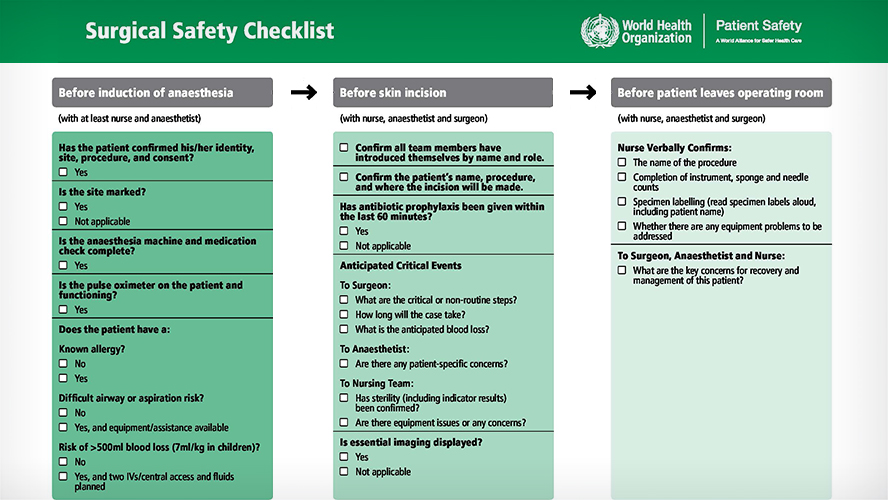
The WHO Surgical Safety Checklist was developed in 2009. It is a 19-item checklist that aims to promote communication and serve as a memory aid for surgical teams.




