
Stay-at-home directives and physical distancing guidelines have changed how we live. But did they help curb the spread of SARS-CoV-2? A new study led by Affiliate Scientist Dr. Sheila Riazi at Toronto General Hospital Research Institute sheds light on how different countries’ public health actions and economic factors have influenced COVID-19’s impact around the world.
The study published in The Lancet's EClinicalMedicine, found that countries with higher caseloads had a higher median population age (ie, a more aged population), a higher prevalence of obesity and took longer to close their borders after the first reported case.
More deaths and more critical cases due to COVID-19 per capita were associated with a higher prevalence of obesity and income inequality, as well as lower numbers of nurses per capita. Surprisingly, countries with higher gross domestic product (ie, the value of a country’s goods and services in proportion to its population) also had more critical cases and higher mortality.
In summarizing the results, Dr. Riazi comments, "What we found is that a country's social and economic policies were as important, if not more so, than the public health measures taken to mitigate COVID-19.”
Fewer COVID-19 diagnoses and faster recovery rates were associated with rapid public health responses such as travel restrictions, nation-wide physical distancing and the closure of non-essential services. While these measures helped hospitals stay within their capacity to treat patients, they were not associated with reducing mortality.
The team analyzed publicly available data from 50 countries. They looked at the type and timing of public health measures as well as social and economic readouts, such as the Global Health Security (GHS) Index. GHS scores are higher for countries such as Canada that have the resources and health system to contain the spread of infection and employ early testing and reporting. The findings revealed that countries with higher GHS scores tended to have higher numbers of recovered cases.
"In Canada, there was early support for testing, which helped to ensure that we maintained sufficient capacity to treat patients with COVID-19. Resources and financial policies were also put in place to support people so they could stay at home," Dr. Riazi explains.
Ongoing research is necessary to continue to weigh the benefits and drawbacks of these measures. This is critical as policymakers navigate the safe reopening of regional and national economies, particularly because it may take two to three weeks to see the full effects of certain public health actions on community transmission.
This study provides critical early insight into the effect of public health measures on reducing the spread of a new virus. In particular, the results indicate that preparing economies and health systems for future threats, including a second wave of COVID-19, is key to saving lives.
Chaudhry R, Dranitsaris G, Mubashir T, Bartoszko J, Riazi S. A country level analysis measuring the impact of government actions, country preparedness and socioeconomic factors on COVID-19 mortality and related health outcomes. EClinicalMedicine. 2020 Jul 21 doi: 10.1016/j.eclinm.2020.100464
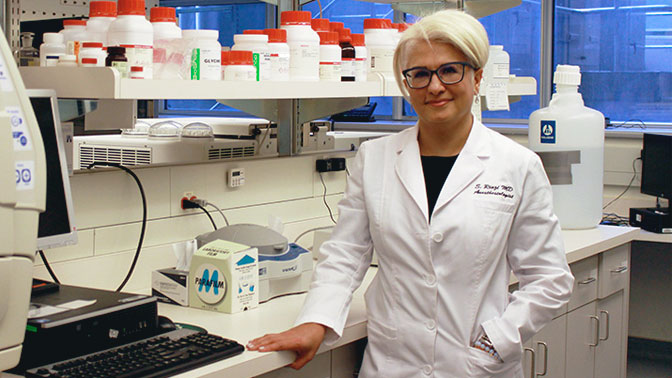
Dr. Sheila Riazi, an Anesthesiologist at UHN’s Toronto Western Hospital and Affiliate Scientist at Toronto General Hospital Research Institute, led the research team.

(L-R) Coauthors Dr. Rabail Chaudhry, Resident Physician, and Dr. Justyna Bartoszko, Assistant Professor, in the Department of Anesthesiology and Pain Medicine at the University of Toronto. Dr. Bartoszko is also a Staff Anesthesiologist at Toronto General Hospital.




