Home page Description:
Gut bacteria help the antidiabetic medication metformin lower blood sugar in rodents.
Posted On: October 25, 2017

Image Caption:
Although individuals with diabetes can lower their glucose through diet and exercise, many still require insulin injections or anti-diabetic medications such as metformin.
Researchers at the Toronto General Hospital Research Institute and Princess Margaret Cancer Centre have discovered that gut bacteria may play a key role in the function of metformin, the most widely prescribed type 2 diabetic medication. They found that the drug alters gut bacteria, which in turn drives a major signalling pathway in the small intestine to lower blood sugar.
The team, led by TGHRI Senior Scientist Dr. Tony Lam, his Ph.D. student Ms. Paige Bauer and former Banting fellow Dr. Frank Duca, used high-fat diet rodents to discover how metformin alters a specific family of bacteria commonly found in the upper small intestine. The bacteria, in turn, impact a glucose-SGLT1 regulating pathway in the intestine to lower glucose or sugar production.
"Metformin is the most widely prescribed type 2 diabetic medication, but its mechanism of action is not understood" says Ms. Bauer, a Ph.D. student in the Department of Physiology at the University of Toronto. She adds that dissecting the mechanism of metformin action can help researchers identify and develop alternative but effective treatments for diabetes, an important goal given that about 25% of patients suffer from metformin-associated side effects such as weakness, stomach pain and nausea.
Using a rodent experimental model, the researchers found that a high-fat diet reduces the amount of Lactobacillus bacteria in the small intestine, and disrupts the SGT1 signalling pathway, which is important for regulating and stabilizing blood sugar. However, metformin treatment restores the amount of Lactobacillus bacteria in the upper small intestine and activates the vital SGLT1 signalling pathway.
Additional experiments were conducted to confirm whether the bacteria could be directly implicated in lowering sugar levels. To do this, the researchers transplanted bacteria from the intestine high-fat diet fed rodents treated with metformin, to rodents under identical conditions that were not treated with metformin. The results showed an increase in Lactobacillus bacteria in the intestine could restore function to the SGLT1 pathway.
The research team is now experimenting with the Lactobacillus bacteria to see which specific species from that group of bacteria can exert similar beneficial changes in signalling pathways that regulate blood sugar stabilization.
“Previous laboratories have correlated metformin action to changes in the gut microbiota in both rodents and humans,” notes Dr. Lam, who holds The John Kitson McIvor Endowed Chair in Diabetes Research and the Canada Research Chair in Obesity, and is also Full Professor of Physiology and Medicine at the University of Toronto.
“The current study reports for the first time a mechanism in the upper small intestine that links changes of the gut microbiota incurred by metformin to the lowering of blood glucose in rodents.”
Dr. Lam emphasized that the clinical relevance of this linking mechanism remains to be investigated in humans.
Other researchers involved in the studies include Drs. T.M. Zaved Waise, Brittany A. Rasmussen, Mona A. Abraham, Helen J. Dranse, from the Toronto General Hospital Research Institute, and Ms. Akshita Puri and Dr. Catherine A. O’Brien from the Princess Margaret Cancer Centre.
This work was supported by the Canadian Institutes of Health Research and the Toronto General & Western Hospital Foundation. TK holds a Tier I Canada Research Chair in Obesity.
Bauer PV, Duca FA, Waise TMZ, Rasmussen BA, Abraham MA, Dranse HJ, Puri A, O’Brien CA, Lam TKT. Metformin Alters Upper Small Intestinal Microbiota that Impact a Glucose-SGLT1-Sensing Glucoregulatory Pathway. Cell Metab. 2017 Oct. doi.org/10.1016/j.cmet.2017.09.019
Source: UHN.ca
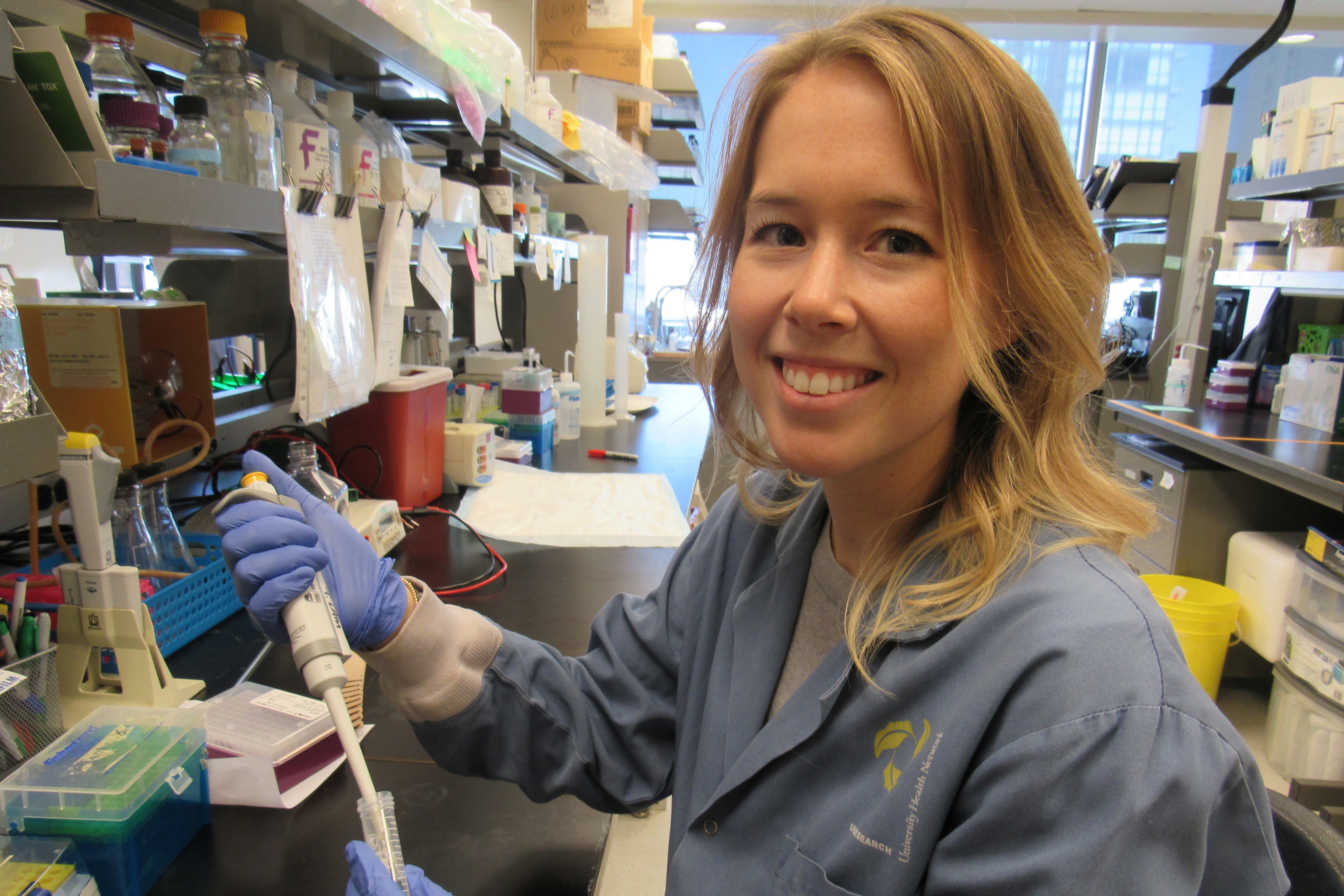
Paige Bauer, Ph.D. student in the lab of Dr. Tony Lam and in the Department of Physiology at the University of Toronto, designed a series of experiments with the Lam lab team to determine how metformin lowers blood sugar through changes in gut bacteria. (Photo: UHN)




