As many hospitals deploy initiatives to reduce preventable harm, the key goal is to strive to minimize errors and improve patient safety.
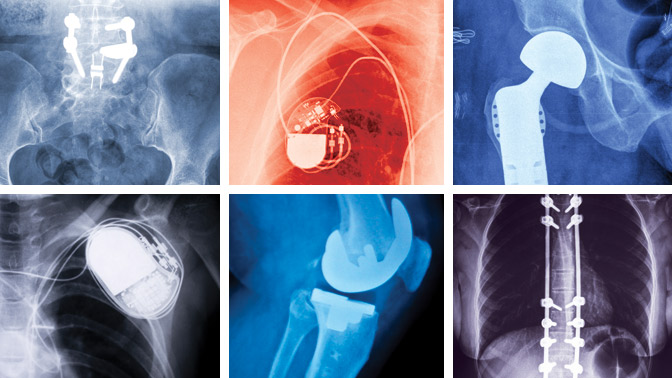
While medical devices such hip, knee and cardiovascular implants are essential to the treatment and well-being of patients—they extend life and improve quality of life—they sometimes don’t work as intended and those incidents may result in harm to the patient.
New research from TGHRI Scientist Dr. Anna R Gagliardi reveals that hospitals may need to improve the systems by which physicians, the health care professionals who implant medical devices, identify and report medical device incidents.
Previous work by Dr. Gagliardi and colleagues analyzed data from Health Canada on medical device recalls over a ten-year period (2005 to 2014) and found that 5% of over 7,200 medical devices recalled were due to problems with the device that could cause harm to patients. Thus, while medical device incidents might be rare events, it is crucial to quickly identify and report such problems.
To further explore the underlying reasons for this underreporting of medical device incidences, Dr. Gagliardi, along with collaborators at UHN, the University of Toronto and across Canada, conducted a qualitative study—one in which detailed information is gathered from a small group of individuals who represent the views and experiences of a larger group. In this case, detailed interviews were conducted with a diverse group of 22 physicians from across Canada.
During the 30 minute interviews, physicians were asked to describe a recent event in which a medical device malfunctioned, the implications, and how they reported it, including any factors that influenced reporting.
The findings showed that there are two factors that could be addressed at the health system level: physician beliefs and health care system capacity. Reporting may be limited by physicians’ understanding of what is and is not a medical device incident. It is further limited by a lack of administrative tools at hospitals to capture the information or bypass purchasing agreements with medical device manufacturers in order to purchase alternative devices.
“Taken together, the results of our study suggest that effective solutions to the underreporting problem must be multifaceted. Rather than simply educating physicians on how and when to report incidents, we need to create the right environment for reporting. This includes the right policies at hospitals, including information systems and incentives to encourage reporting. It may also include establishment of national and international systems to broadly capture and publicly share information about medical device incidents,” says Dr. Gagliardi.
This work was supported by the Canadian Institutes of Health Research and the Toronto General & Western Hospital Foundation.
Gagliardi AR, Takata J, Ducey A, Lehoux P, Ross S, Trbovich PL, Easty A, Bell CM, Urbach DR. Medical Device Recalls in Canada from 2005 to 2015. Int J Technol Assess Health Care. 2017 Sep 18. doi: 10.1017/S0266462317000824.
Gagliardi AR, Ducey A, Lehoux P, Turgeon T, Ross S, Trbovich P, Easty A, Bell C, Urbach D. Factors influencing the reporting of adverse medical device events: qualitative interviews with physicians about higher risk implantable devices. BMJ Qual Saf. 2017 Aug 2. doi: 10.1136/bmjqs-2017-006481.

Dr. Anna Gagliardi, Scientist at Toronto General Hospital Research Institute, is the lead author of the study, which identifies the factors that influence whether physicians identify and report medical device incidents.




