Home page Description:
Protein is associated with alterations in blood flow in early diabetes-related eye damage.
Posted On: November 23, 2016
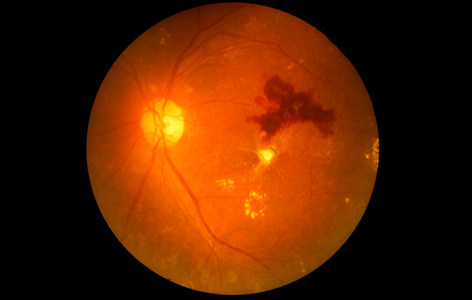
Image Caption:
Virtually everyone who has had diabetes for at least 20 years will suffer from some form of vision impairment caused by damage to retinal blood vessels (pictured).
Diabetic retinopathy is the most common cause of blindness in working-age adults. It is a serious complication of diabetes in which the tissue layer at the back of the eye (retina) deteriorates.
Blood flow in the retina is altered in the early stages of diabetic retinopathy, suggesting that it could be a predictor of future vision loss; however, why blood flow alterations occur in people with the disease and how it contributes to degeneration of the retina is not known.
To address this issue, Krembil Senior Scientist Dr. Christopher Hudson and a team of graduate students and colleagues initiated a study to identify which proteins influence retinal blood flow in people with diabetic retinopathy. Using samples of eye fluid collected from study participants with early-stage diabetic retinopathy, his research team measured the levels of specific proteins that are thought to be disturbed in early diabetes. They found that people with diabetic retinopathy have increased levels of two proteins, TGF-β and PLGF, and decreased levels of the FGF-1 protein.
The team noted that it was the decreased levels of FGF-1 in particular that were associated with decreased retinal blood flow.
“Our study is the first to implicate FGF-1 as a factor associated with changes in retinal blood flow found in people with early diabetic retinopathy,” explains Dr. Hudson. “Although more research is needed, we are one step closer to developing a test that can help predict who is at risk of developing the disease—enabling earlier treatments to prevent or reverse vision loss.”
This work was supported by the Ontario Ministry of Research, Innovation and Science, the University of Toronto, the National Institutes of Health and the Toronto General & Western Hospital Foundation.
Aqueous humour concentrations of TGF-β, PLGF and FGF-1 and total retinal blood flow in patients with early non-proliferative diabetic retinopathy. Khuu LA, Tayyari F, Sivak JM, Flanagan JG, Singer S, Brent MH, Huang D, Tan O, Hudson C. Acta Ophthalmologica. doi: 10.1111/aos.13230. 2016 Sep 28. [Pubmed abstract]
Blood flow in the retina is altered in the early stages of diabetic retinopathy, suggesting that it could be a predictor of future vision loss; however, why blood flow alterations occur in people with the disease and how it contributes to degeneration of the retina is not known.
To address this issue, Krembil Senior Scientist Dr. Christopher Hudson and a team of graduate students and colleagues initiated a study to identify which proteins influence retinal blood flow in people with diabetic retinopathy. Using samples of eye fluid collected from study participants with early-stage diabetic retinopathy, his research team measured the levels of specific proteins that are thought to be disturbed in early diabetes. They found that people with diabetic retinopathy have increased levels of two proteins, TGF-β and PLGF, and decreased levels of the FGF-1 protein.
The team noted that it was the decreased levels of FGF-1 in particular that were associated with decreased retinal blood flow.
“Our study is the first to implicate FGF-1 as a factor associated with changes in retinal blood flow found in people with early diabetic retinopathy,” explains Dr. Hudson. “Although more research is needed, we are one step closer to developing a test that can help predict who is at risk of developing the disease—enabling earlier treatments to prevent or reverse vision loss.”
This work was supported by the Ontario Ministry of Research, Innovation and Science, the University of Toronto, the National Institutes of Health and the Toronto General & Western Hospital Foundation.
Aqueous humour concentrations of TGF-β, PLGF and FGF-1 and total retinal blood flow in patients with early non-proliferative diabetic retinopathy. Khuu LA, Tayyari F, Sivak JM, Flanagan JG, Singer S, Brent MH, Huang D, Tan O, Hudson C. Acta Ophthalmologica. doi: 10.1111/aos.13230. 2016 Sep 28. [Pubmed abstract]

