The best defence is a good offence. This adage, often applied to sports or military strategies, suggests that attacking one’s opponent offers the greatest protection. Researchers and clinicians are taking this approach to fight cancer—developing powerful new therapies that seek out and kill cancer cells.
One such approach is immune therapy: it works by boosting the number and activity of tumour-infiltrating lymphocytes (TILs), immune cells that go on the offensive by migrating into tumours to target and destroy them. Although this strategy holds promise, challenges remain because certain tumours have developed defence mechanisms that block TIL activity.
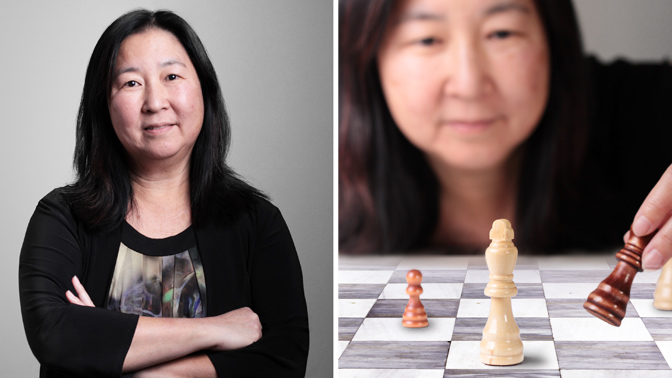
These tumours, however, are no match for Dr. Pamela Ohashi. She is a pioneer in figuring out how the immune system interacts with cancer in order to develop new immune therapies.
In an article published in the prestigious journal Nature Medicine, Dr. Ohashi and her research team, including Dr. Sarah Crome, revealed that an internal battle may be going on: they found that certain ovarian tumours contain other immune cells, called regulatory innate lymphoid cells (ILCregs), that block the activity of cancer-fighting TILs. The ILCregs did this in two ways: they reduced the ability of TILs to grow and multiply, and altered the ability of the TILs to attack cancer cells.
The team also found that the tumours from some patients contained ILCregs, while those from others did not, suggesting that some tumours may be able to attract or promote growth of ILCregs.
Immune therapies work by helping the immune system to target and kill cancer."
“By looking at tumour biology from this different perspective, we have a better understanding of the barriers that prevent a strong immune response,” explains Dr. Ohashi. “Our research reveals a promising new strategy to develop combined therapies that simultaneously target ILCregs while promoting TIL growth and function—delivering a stronger ‘one-two punch’ against the disease.”
Building on these findings, her team is now developing a test to identify ILCregs in patients, which may help predict whether the patient will respond to immune therapy. Dr. Ohashi says, “This knowledge would help doctors and patients make more informed medical decisions, personalize cancer treatment and ultimately improve the effectiveness of immune therapies.”





