
Millions of photoreceptor cells in the eye are responsible for converting light into signals that can be transmitted to the brain and processed. When these cells malfunction or are damaged, vision loss often results.
Laboratory tests over the past two decades have shown that when photoreceptors are transplanted into the retina (i.e., the light-sensitive layer of tissue at the back of the eye) vision loss can be reversed. Dr. Valerie Wallace, Co-Director and Senior Scientist at the Donald K. Johnson Eye Institute, and her research team have observed a phenomenon that helps explain how these cells restore vision.
“Transplanted cells rarely integrate into the retina, yet they are somehow still able to rescue vision,” says Dr. Arturo Ortin-Martinez, a Scientific Associate in Dr. Wallace’s lab and the lead author of the study. “Understanding this process will enable us to improve the success of transplants.”
The researchers found that donor cells form microscopic, tunnel-like bridges—called nanotubes—with the host photoreceptors. Materials that are essential to photoreceptor function can move between the cells via these nanotubes.
Using microscopy techniques that can track proteins and other components of cells, the team observed the nanotubes forming and extending as protrusions from the donor cells towards the recipient cells. They then saw materials moving between the cells.
Among the techniques used to gain this insight was an exciting method developed by Dr. Wallace’s group called InVision. This method makes eye tissue transparent, enabling researchers to image whole eyes, rather than thin sections of tissue. After examining the eye at this scale, the team concluded that around 80% of the donated photoreceptors formed nanotubes with host photoreceptors.
A 3D reconstruction of immunofluorescence images captured from a whole, intact eye that was prepared using the InVision method. Donor and host photoreceptors (green) are localized in the same region and are connected by nanotubes. |
When tracking the movement of cellular materials, the researchers found that the amount of material transferred to the host cells depended on the persistence of the donor cells—more material was transferred when the cells survived longer. The research team also discovered that materials were only transferred when the donor cells were photoreceptors; materials were rarely transferred from other types of cells, such as brain neurons.
“We think that this exchange helps restore vision in transplant recipients by supplying materials that are missing in the damaged retina,” says Dr. Wallace. “Next we need to explore what cargo is moving between cells and how we can optimize the transfer process.”
Because photoreceptors are a type of nerve cell, these new observations may impact the design of cell-based strategies for treating degeneration in other parts of the nervous system.
This work was supported by the Ontario Institute of Regenerative Medicine, Medicine by Design at the University of Toronto, the Krembil Foundation and the UHN Foundation. V Wallace holds a Tier 1 Canada Research Chair in Retina Regeneration.
Ortin-Martinez A, Yan NE, Tsai ELS, Comanita L, Gurdita A, Tachibana N, Liu ZC, Lu S, Dolati P, Pokrajac NT, El-Sehemy A, Nickerson PEB, Schuurmans C, Bremner R, Wallace VA. Photoreceptor nanotubes mediate the in vivo exchange of intracellular material. EMBO J. 2021 Sep 8. doi: 10.15252/embj.2020107264.
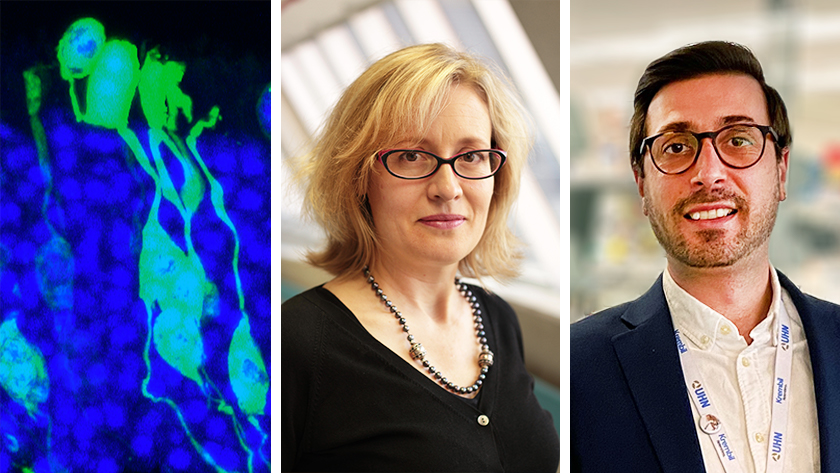
Left: Immunofluorescence image showing protein (green) being transferred between donor (top) and recipient (bottom) photoreceptor cells. Centre: Dr. Valerie Wallace is the Donald K. Johnson Chair in Vision Research at UHN. Right: Dr. Arturo Ortin-Martinez is the first author of the study and a Scientific Associate in Dr. Wallace’s lab.




