A team of researchers at UHN’s Princess Margaret Cancer Centre (PM) has developed a comprehensive way to map the ability of molecules on the surface of cancer cells to serve as immunotherapy targets.
“Immunotherapy is quickly becoming a gamechanger, and is now considered—along with surgery, radiotherapy and chemotherapy—a cornerstone in the fight against cancer,” says Dr. Naoto Hirano, Senior Scientist at PM. “However, a major drawback of current immunotherapies is that they often only work in a fraction of patients. It is also very difficult to predict which patients will benefit.”
To overcome this limitation, the research team—including postdoctoral fellows Kenji Murata and Munehide Nakatsugawa—developed a technique that greatly expands how immunotherapy targets cancer so that more people might benefit from the treatment.
In cancer immunotherapy, certain immune cells—known as killer T cells—are temporarily isolated from patients. They are then ‘taught’ to target certain features, known as antigens, on the surface of cancer cells. In order for T cells to recognize these antigens, the antigens must be chopped into fragments called peptides and loaded onto a larger molecule known as type I human leukocyte antigen (HLA) complex, of which there are many different types.
The T cells are then injected back into patients and, if the immunotherapy is successful, begin to seek out and destroy the cancer cells.
Currently, immunotherapy targeting is limited. Only a few types of HLAs are used, which are found in only a subset of people and ethnic groups. Furthermore, only a select number of peptides, which are present in a fraction of the cancer cells, are used.
To address this, and to increase the diversity of targeting approaches, the researchers used immune cell samples from eight different individuals with melanoma. Using these samples, and a new streamlined approach, they were able to test the ability of 25 different types of HLAs and 800 different peptides to target the cancer.
The researchers also identified potent new peptides derived from well-established cancer antigens—called MART1 and NY-ESO1—that are present on a wider number of cancer cells than currently used antigens.
“By expanding the diversity of targeting approaches, our strategy allows for a more complete examination of the immune response. It opens the door for the development of immunotherapies that are effective in a broader group of patients,” concludes Dr. Hirano.
To read more, see the press release. The research study was supported by the Ontario Institute for Cancer Research, The Princess Margaret Cancer Foundation, Mitacs, the Province of Ontario, and the Natural Sciences and Engineering Research Council of Canada.
Landscape mapping of shared antigenic epitopes and their cognate TCRs of tumor-infiltrating T lymphocytes in melanoma. Murata, K, ..., Naoto, H. eLife 2020;9:e53244 doi: 10.7554/eLife.53244.
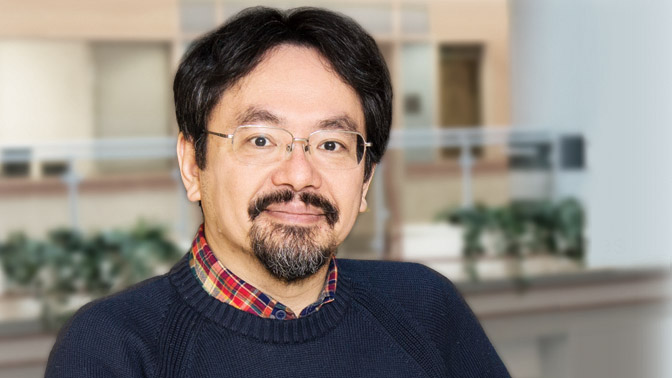
Dr. Naoto Hirano (pictured) is lead author of the study and a Senior Scientist at the Princess Margaret Cancer Centre.




