Anyone who has played the 80s board game Mouse Trap will remember how a chain reaction that starts with a small ball rolling side-to-side down a hill ends with a mouse being trapped under a plastic net.
Just like how different events in the game come together to set the trap, different and sometimes unlikely parts of the body can conspire in the development of disease.
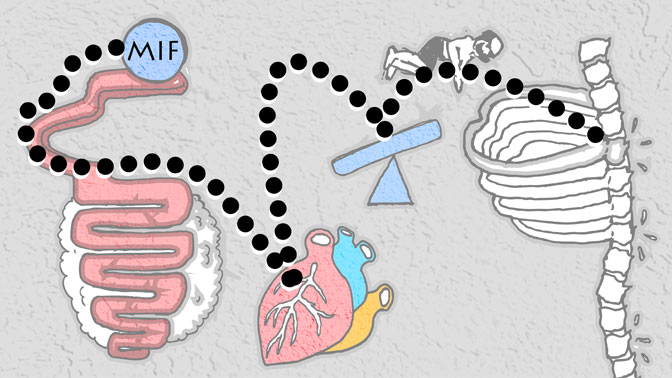
Recent findings from Krembil Scientist Dr. Nigil Haroon have identified a molecule, known as macrophage migration inhibitory factor (MIF), which may link inflammation in the gut and a type of spinal arthritis known as ankylosing spondylitis (AS).
The link between the gut and AS is well known, as over half of those with AS also have bowel inflammation; however, it is still unknown how the gut might contribute to the disease, if at all.
Dr. Haroon’s team focused on MIF, because it is elevated in the blood of patients with AS and other inflammatory diseases, such as psoriasis and inflammatory bowel diseases.
By analyzing clinical data, the researchers revealed that elevated MIF levels could be used to predict the progression of AS. Specifically, they found that MIF can promote inflammation and bone formation in the spine—two hallmarks of AS. Dr. Haroon comments, “We found that MIF can directly mediate bone formation in experimental models involving bone-forming cells known as osteoblasts, and that MIF does this by modulating a cell signalling pathway known as Wnt.”
Another question that the research team explored was: where in the body does MIF originate from?
It was this question that led them to the gut. Initially the researchers looked to circulating immune cells—obvious culprits, as they are involved in inflammation—however, they were unable to find heightened MIF stores in these cells.
Next, they explored whether tissues in the large intestine might be the source. The results revealed, for the first time, that cells of the small intestine known as Paneth cells, as well as ‘resident’ immune cells in the same tissue, known as CD68+ macrophages, produce MIF.
“These results led us to propose a new hypothesis: inflamed cells of the gut secrete MIF, perhaps as a response to altered gut microbes, which then travels to the spine where it contributes to the inflammation and irregular bone formation in the joints of the back, ultimately leading to the debilitating pain and stiffness experienced by individuals with ankylosing spondylitis,” says Dr. Haroon.
Future studies will be focused on advancing the use of MIF to predict AS progression, as well as the development of future therapeutics that target MIF to slow or stop progression of the disease.
This work was supported by the Arthritis Society, the Krembil Foundation, the Canadian Institutes of Health Research, and the Toronto General & Western Hospital Foundation.
Macrophage Migration Inhibitory Factor induces inflammation and predicts spinal progression in Ankylosing Spondylitis. Ranganathan V, Ciccia F, Zeng F, Sari I, Guggino G, Muralitharan J, Gracey E, Haroon N. Arthritis Rheumatol. 2017 Jun 8.

The study was led by Krembil Scientist Dr. Nigil Haroon, whose laboratory is located at the Krembil Discovery Tower (pictured).

