Home page Description:
Why diabetic men are more likely to get kidney disease.
Posted On: March 16, 2017
By Shaalee Dworski, ORT Times Writer and UHN Trainee
The burden of kidney disease is heavy and lifelong. Damage to the kidneys is irreversible and can lead to kidney failure, which drastically decreases the quality and length of life.
In Canada, diabetes is the leading cause of kidney disease. Interestingly, men are more likely to develop kidney disease than women. Researchers at UHN hypothesized that male sex hormones may play a role in this sex effect. Recently, Dr. Sergi Clotet, a postdoctoral fellow in Dr. Ana Konvalinka’s laboratory, investigated the effects of male and female sex hormones within the kidney, conducting a thorough investigation from the cell to organ level.
Previous research indicates that in vitro exposure to testosterone stimulates apoptosis in the proximal tubule cells of the kidney, but the specific proteins that mediate this event are unknown. In this work, the authors studied the changes in the proteome of a human kidney proximal tubule cell line when it was exposed to estrogen or dihydrotestosterone (DHT), a testosterone analog that cannot be converted into estrogen. Out of over 5000 proteins identified, short exposure to DHT resulted in a significant change of expression in 60 proteins.
A significant number of the proteins changed by DHT exposure are involved in biological processes related to energy metabolism, such as glucose metabolism, hexosamine biosynthetic pathway and fatty acid oxidation. These processes are known to play a critical role in the context of diabetic kidney disease. Therefore, the authors decided to validate their proteomic findings not only in their in vitro system, but also in two different animal experimental models of diabetes.
They observed that three of the proteins -- —GPI, GNPNAT1, and HADHA --— are elevated in the kidneys of male diabetic mice murine models compared to females. In agreement, they also observed increased oxidative stress in the kidneys of diabetic and non-diabetic males mice compared to females in the experimental model.
This study identifies for the first time the effects of sex hormones on the proteome of human renal proximal tubule cells. With their findings, the authors propose a novel link between male sex hormones and altered renal energy metabolism that may help to understand the more rapid kidney disease progression observed in male patients.
Future treatments could be based on ameliorating the negative effects of male sex hormones on the renal proximal tubular cell homeostasis in order to reduce kidney damage in male patients.
The article is available here (link is external).
The ORT Times spoke with first author, Dr. Sergi Clotet.
1. Are males at an increased risk of other diabetes-related pathology?
Interestingly, previous studies have shown that DHT is capable of inducing apoptosis in pancreatic beta-cells (the cells responsible of producing insulin), and that male sex increases the severity of not only diabetic nephropathy, but also diabetes per se. However, among all other diabetic complications, robust and consistent sex differences have not been reported.
The burden of kidney disease is heavy and lifelong. Damage to the kidneys is irreversible and can lead to kidney failure, which drastically decreases the quality and length of life.
In Canada, diabetes is the leading cause of kidney disease. Interestingly, men are more likely to develop kidney disease than women. Researchers at UHN hypothesized that male sex hormones may play a role in this sex effect. Recently, Dr. Sergi Clotet, a postdoctoral fellow in Dr. Ana Konvalinka’s laboratory, investigated the effects of male and female sex hormones within the kidney, conducting a thorough investigation from the cell to organ level.
Previous research indicates that in vitro exposure to testosterone stimulates apoptosis in the proximal tubule cells of the kidney, but the specific proteins that mediate this event are unknown. In this work, the authors studied the changes in the proteome of a human kidney proximal tubule cell line when it was exposed to estrogen or dihydrotestosterone (DHT), a testosterone analog that cannot be converted into estrogen. Out of over 5000 proteins identified, short exposure to DHT resulted in a significant change of expression in 60 proteins.
A significant number of the proteins changed by DHT exposure are involved in biological processes related to energy metabolism, such as glucose metabolism, hexosamine biosynthetic pathway and fatty acid oxidation. These processes are known to play a critical role in the context of diabetic kidney disease. Therefore, the authors decided to validate their proteomic findings not only in their in vitro system, but also in two different animal experimental models of diabetes.
They observed that three of the proteins -- —GPI, GNPNAT1, and HADHA --— are elevated in the kidneys of male diabetic mice murine models compared to females. In agreement, they also observed increased oxidative stress in the kidneys of diabetic and non-diabetic males mice compared to females in the experimental model.
This study identifies for the first time the effects of sex hormones on the proteome of human renal proximal tubule cells. With their findings, the authors propose a novel link between male sex hormones and altered renal energy metabolism that may help to understand the more rapid kidney disease progression observed in male patients.
Future treatments could be based on ameliorating the negative effects of male sex hormones on the renal proximal tubular cell homeostasis in order to reduce kidney damage in male patients.
The article is available here (link is external).
The ORT Times spoke with first author, Dr. Sergi Clotet.
1. Are males at an increased risk of other diabetes-related pathology?
Interestingly, previous studies have shown that DHT is capable of inducing apoptosis in pancreatic beta-cells (the cells responsible of producing insulin), and that male sex increases the severity of not only diabetic nephropathy, but also diabetes per se. However, among all other diabetic complications, robust and consistent sex differences have not been reported.
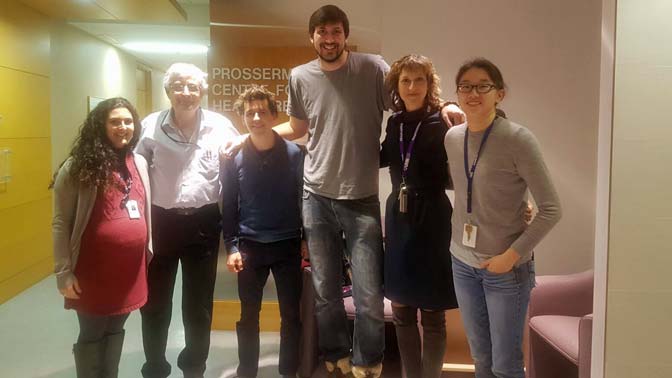
From left to right: Stella Vasiliou,Dr. Eleftherios Diamandis, Dr. Igor Batruch, Dr.Sergi Clotet, Dr. Ana Konvalinka, Julie Van.




